What is healthcare interoperability?
Healthcare interoperability is like a universal language that allows different systems — such as mobile apps, third-party applications, and EHR or EMR platforms — to communicate effectively. These systems utilize Health Information Exchange (HIE) standards, data integration architectures, application programming interfaces (APIs), and standardized information formats. Without this common language, critical information would remain siloed, making it difficult for healthcare providers to access the data they need. Just as two people speaking different languages need a translator to communicate, EHR/EMR solutions require health interoperability standards to share data seamlessly.
On the other hand, interoperability supports payers and health systems in their risk management and compliance strategies. By enabling rapid data exchange, interoperability helps to monitor and manage risks more effectively. For instance, interoperability aids in tracking patient outcomes, adverse events, and readmission rates, providing valuable insights for improving care quality and reducing risks. Additionally, it ensures that data sharing practices comply with regulatory requirements such as HIPAA or GDPR, safeguarding patient privacy and security. Through better data integration and analysis, payers and health systems can enhance their strategic planning, resource allocation, and overall operational efficiency.
What data is exchanged via interoperable systems?
Health information technology systems that adhere to the United States Core Data for Interoperability (USCDI v1) standards can exchange a wide range of information. This includes demographic details, vital signs, smoking status, medications, lab results, clinical notes, allergies, and intolerances, among other data. By incorporating HL7 interoperability standards, these systems ensure that the exchanged information is not only comprehensive but also standardized, facilitating efficient communication between different healthcare entities.
Benefits of implementing data Interoperability standards in healthcare
Healthcare relies heavily on having the right data at the right time. Adopting interoperability in medical practice positively influences diagnosis, treatment, ongoing care, and patient outcomes.
Here are several examples of interoperability achieved through FHIR implementation:
Easy access to patient data
Patients often visit multiple healthcare providers, including hospitals, urgent care centers, pharmacies, laboratories, and solo practitioners. Without interoperability, they must carry their health records or repeatedly provide their medical history, leading to potential data loss or inaccuracies. This fragmentation negatively impacts the continuity of care and can be critical in emergencies when every second counts.
FHIR implementation secures accessible data and provides a comprehensive and clear picture of patient data, guiding balanced medical decisions, better treatment, and resource savings. Clinicians can immediately access a patient’s complete history, and even clinical genomics, allowing them to continue treatment seamlessly from where the previous provider left off.
Reduction of costs
FHIR data and document query implementation guides interoperability efforts, resulting in significant cost savings. By reducing redundant procedures due to inaccessible patient information, interoperability can save up to $3 billion annually. It also minimizes the time clinicians spend manually entering reference data, improving productivity and organizational workflows.
Fewer medical errors
Lack of real-time access to medical history or lab results can pose significant health risks. Interoperability plays a crucial role in ensuring the high accuracy of bulk data, eliminating human error, and reducing the risk of mistakes. With the implementation of FHIR, records transferred across different applications adhere to international healthcare data standards. This standardization guides the data structure, ensuring that the content is correctly interpreted, ultimately enhancing patient care and safety
Accurate public health data
By connecting internal software to healthcare networks used for research, providers can aid scientists in studying treatment and medication effectiveness. Full data visibility helps prevent or mitigate epidemiological outbreaks, allowing researchers to evaluate health crises, find effective solutions, and quickly communicate this information to healthcare organizations.
Why was FHIR created?
FHIR, or Fast Healthcare Interoperability Resources, was developed in 2012 by a team of health information technology implementers led by Grahame Grieve. The team aimed to create a modern approach to health information exchange by combining the simplicity of existing methods with the power of Internet technologies.
The objective was to develop a standard that would be user-friendly for software developers while promoting interoperability and simplifying application creation in the healthcare market. To achieve this, FHIR incorporates modern technologies such as JSON, XML, HTTP, and OAuth, alongside existing exchange methods like HL7 v2 messages and Clinical Document Architecture (CDA).
The goal of FHIR is to ensure seamless integration with existing workflows and systems by building on established standards like HL7 v2 and CDA. This approach allows FHIR to provide compatibility with legacy systems, facilitating a smooth transition to the new standard while embracing modern healthcare information exchange methods.
Who is adopting FHIR?
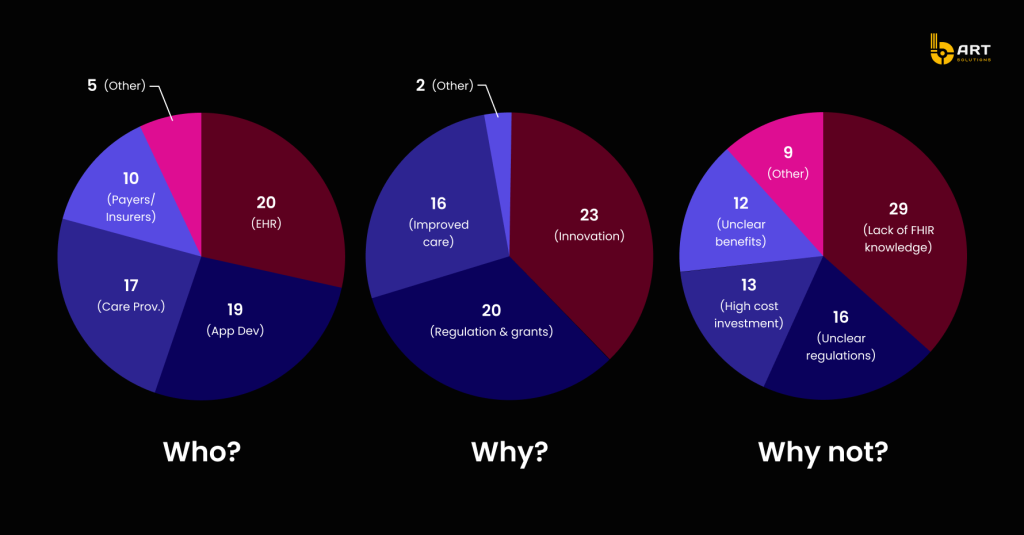
The adoption of FHIR is prominent among EHR vendors, app developers, and care providers, with additional interest from health information systems, jurisdictional assets/repositories, national services, eHealth agencies, researchers, and individual companies and hospitals.
The primary reasons for adopting FHIR include innovation and compliance with regulations and grants. Additionally, improved data analytics, reporting capabilities, and ease of implementation are also significant factors. Many respondents acknowledge the role of patient advocacy in driving healthcare data availability, with a notable focus on health data standards.
6 examples of HL7 FHIR implementation
- Personal Health Record Management: Managing and accessing personal health records across various healthcare providers can be fragmented and challenging for patients. FHIR implementation enables seamless health data exchange, allowing patients to aggregate and access their personal information more easily. With standardized data formats and APIs, patients can view their health data from multiple sources, improving care coordination and informed decision-making.
- Healthcare Document Sharing: Sharing healthcare documents, such as medical records, between institutions and providers can be slow, cumbersome, and error-prone. FHIR streamlines document sharing by providing a structured and standardized format for healthcare documents, ensuring that critical information is accurately and efficiently exchanged between different systems.
- Clinical Decision Support: Healthcare professionals often face information overload when making clinical decisions and need quick access to evidence-based guidelines and patient-specific data. FHIR enhances clinical decision support systems by structuring patient data, allowing these systems to integrate seamlessly with EHRs. This provides real-time, relevant information to aid healthcare providers in making informed decisions, ultimately improving patient safety and care.
- Public Health Surveillance: Public health organizations require timely and accurate data to monitor disease outbreaks, track health trends, and respond to health emergencies. FHIR standardizes public health data exchange, making it easier for healthcare facilities to report relevant data to public health authorities. This streamlines surveillance and response efforts, enabling quicker interventions and better population health management.
- Clinical Research: Clinical research involves collecting, aggregating, and analyzing data from various sources, which can be time-consuming and error-prone. FHIR facilitates data sharing between research institutions, EHRs, and other systems. This enables researchers to access structured data from diverse sources, accelerating the research process and supporting advancements in medical science.
- Patient Engagement: Engaging patients in their own healthcare and treatment plans is crucial but can be challenging when providing accessible and understandable health information. FHIR promotes patient engagement by enabling the development of user-friendly healthcare apps and portals. Patients can access their health data, receive personalized health information, and actively participate in their care, leading to better health outcomes.
How to implement FHIR?
FHIR provides a flexible framework with various implementation options to meet the specific needs of healthcare organizations.
FHIR RESTful API Implementation
This approach uses web standards to perform Create, Read, Update, and Delete (CRUD) operations on resources through RESTful APIs. It is particularly valuable for real-time applications that require dynamic interactions among healthcare systems. Resources are treated as URLs, and standard HTTP verbs are used, making the implementation straightforward. RESTful API implementation is favored for its simplicity, scalability, and compatibility with modern web architectures.
FHIR messaging implementation
In this method, FHIR resources are integrated into existing HL7 message structures, allowing healthcare systems to benefit from FHIR’s granularity and flexibility while maintaining investments in HL7 messaging infrastructure. It operates on an event-driven model, where a trigger event in one system initiates the transmission of a message to another system. This approach is suitable for batch-style and background processing tasks.
FHIR document-based implementation
The document-based approach bundles FHIR resources together to form self-contained units of healthcare information known as documents. This is effective for managing complex use cases involving multiple resources, such as discharge summaries or referral notes. These documents can be easily shared, stored, and retrieved, making them ideal for promoting interoperability.
FHIR hybrid implementation
Hybrid implementation combines various approaches to meet the specific needs of the healthcare system. For instance, a healthcare provider might use a RESTful API for real-time interactions, employ messaging for batch processing tasks, and leverage document-based approaches for managing intricate FHIR implementation use cases. This adaptable method ensures that healthcare systems can utilize FHIR’s strengths in alignment with their operational requirements and strategic objectives.
Comparison of FHIR implementation approaches
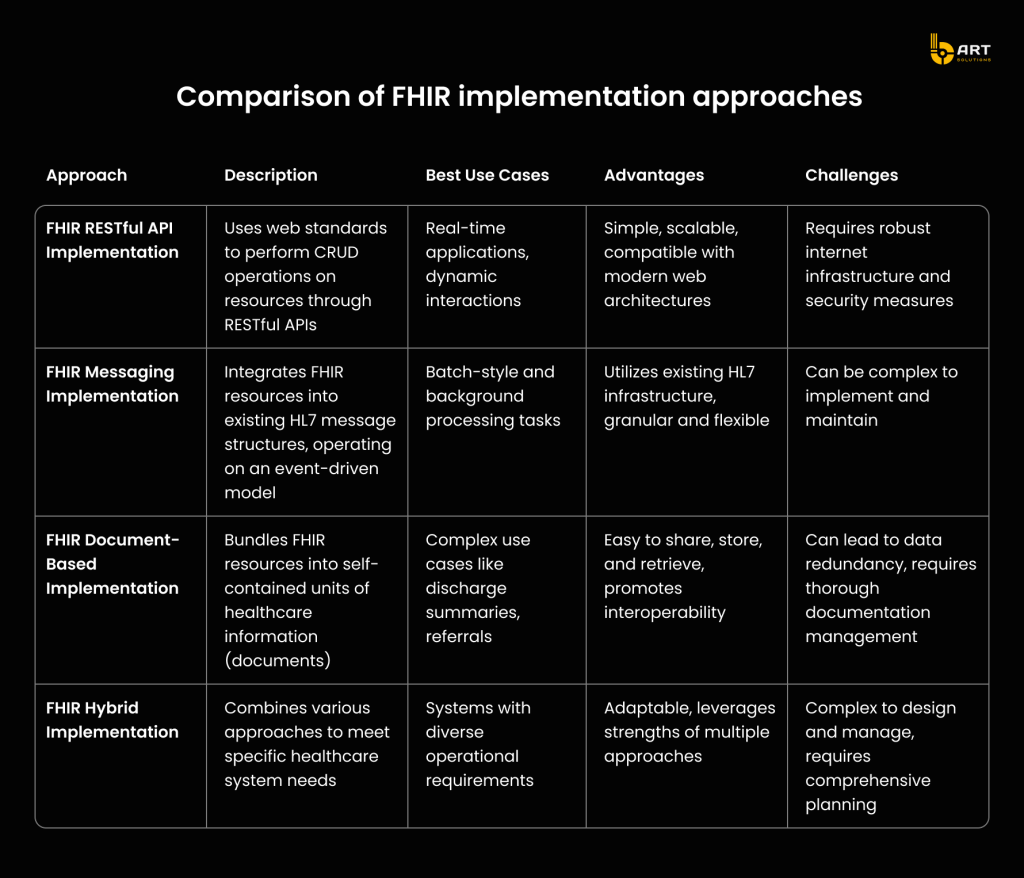
While each FHIR implementation approach has its unique advantages and specific use cases, the FHIR RESTful API implementation stands out as the best approach for modern healthcare systems. Its simplicity, scalability, and compatibility with current web architectures make it ideal for real-time applications and dynamic interactions. The straightforward nature of RESTful APIs reduces the complexity of implementation and maintenance, making it a cost-effective solution.
For expert help in developing FHIR-based healthcare platforms, contact bART Solutions.
FHIR implementation: Step-by-step guide
A professional development team is crucial to the successful implementation of Fast Healthcare Interoperability Resources (FHIR), as their technical expertise directly impacts the efficiency and reliability of healthcare data exchange. These experts design and develop APIs that enable various healthcare systems to communicate seamlessly, ensuring that patient information is consistently accurate and readily available. Beyond development, they also configure systems to comply with healthcare regulations and security standards, safeguarding sensitive patient data from breaches. Additionally, they provide ongoing support, troubleshoot issues, and optimize performance to ensure the smooth functioning of FHIR integrations, ultimately enhancing patient care and operational efficiency in healthcare settings.
Each FHIR-based healthcare project should follow the outlined guide. Keep in mind that this is just an example, and your specific project may require additional steps depending on its complexity.
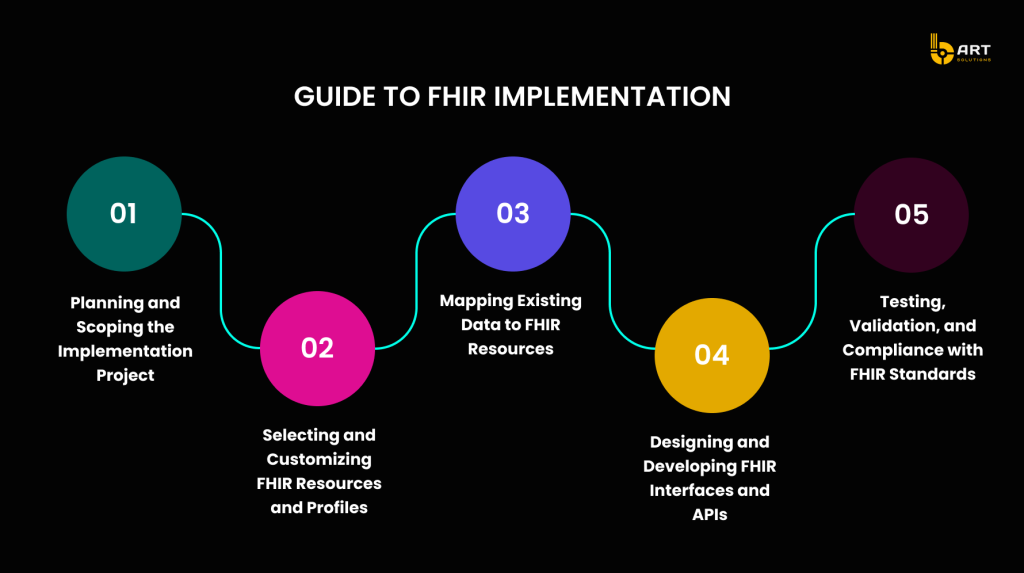
Planning and scoping the implementation
The success of any FHIR project lies in careful planning and a well-defined scope. Development team starts by establishing clear objectives, whether the goal is to enhance interoperability, improve patient data management, or both. They identify key stakeholders, allocate the necessary resources, and develop a realistic timeline with specific milestones. Additionally, they create a risk management strategy to anticipate and address potential challenges, ensuring seamless execution.
Data mapping and transformation
One of the primary responsibilities of tech experts is data mapping and transformation. They map data from legacy systems to the FHIR format, ensuring accurate and efficient translation of information. This process requires a deep understanding of both existing data structures and the FHIR standard.
Developing and integrating APIs
Tech professionals are responsible for designing and developing FHIR APIs and interfaces. This involves creating software interfaces that enable healthcare systems to exchange data using HL7 FHIR standards. Developers must have a thorough knowledge of RESTful API principles and common data formats like XML and JSON. The development process includes ensuring that APIs are user-friendly, secure, and capable of seamless interaction with other systems. This is critical for real-time data exchange and integration across various healthcare platforms.
Ensuring data security
Data security is a paramount concern in healthcare, robust security measures must be implemented to protect data during exchange and storage. This includes encryption, secure authentication protocols, and regular security audits to identify and mitigate vulnerabilities. By ensuring data security, tech team protects patient privacy and builds trust among healthcare stakeholders.
Compliance with regulatory standards
Tech professionals also ensure that FHIR implementations comply with healthcare regulations such as HIPAA in the United States or GDPR in Europe. They continuously monitor and update systems to adhere to the latest standards and guidelines. This involves implementing practices that ensure data handling and sharing are in line with legal requirements.
Optimizing system performance
Optimizing system performance is another critical responsibility of the development team. They conduct regular testing to ensure that FHIR implementations function correctly and efficiently. This includes validating that systems use FHIR resources properly, manage patient data effectively, and communicate seamlessly with other systems. Continuous monitoring and optimization help maintain high performance and reliability, ensuring that healthcare providers can deliver the best possible care.
Supporting continuous improvement
Finally, tech professionals support continuous improvement in healthcare data management. They stay updated with the latest advancements in FHIR standards and technologies, ensuring that implementations remain current and effective. By promoting ongoing education and adaptation, tech experts help healthcare organizations continually enhance their data interoperability capabilities.
At bART Solutions we follow these practices to guarantee a successful FHIR implementation, ushering in a new era of enhanced interoperability and improved patient care in your healthcare setting.
Understanding the cost of FHIR development
The cost of FHIR development depends on several key factors that shape project planning and resource allocation.
Here are the main factors to consider:
- Scope and Complexity: Projects with extensive functionality, intricate data models, or complex integration requirements often require more resources, development time, and specialized expertise, which can increase the overall cost.
- Interoperability Requirements: The level of interoperability needed for your project affects its complexity and cost. Integrating with multiple systems, ensuring data consistency, and adhering to industry standards may incur additional expenses.
- Data Volume and Complexity: Handling large datasets, complex data transformations, data mapping, and validation requirements typically necessitates extra development effort and resources, impacting the overall cost.
- Integration and Customization: FHIR development frequently involves integrating with existing systems and customizing FHIR resources and profiles to meet specific needs. These factors influence development efforts and, consequently, costs.
- Security and Compliance: Implementing robust security measures, adhering to privacy regulations like HIPAA, and maintaining comprehensive audit trails add complexity and cost to the development process.
- Development Team Expertise: Highly skilled developers with deep knowledge of FHIR standards and the healthcare domain may command higher fees. However, their expertise can lead to smoother development and superior outcomes.
- Project Timeline: Projects with accelerated timelines may require additional resources or overtime, potentially increasing expenses.
For a more accurate estimate of the costs of your FHIR solution, consult with our experts in FHIR implementation. They can assess your specific needs, evaluate the project’s scope, and provide tailored insights.
Challenges and considerations in adopting FHIR
Implementing FHIR and interoperability standards is essential for modernizing healthcare systems, but it comes with its own set of challenges.
Here are some common obstacles and insights into overcoming them.
Common challenges in adopting FHIR
- Legacy System Integration: Many healthcare organizations still rely on legacy systems that are not designed to work with modern interoperability standards like FHIR. Integrating these outdated systems with new standards can be complex and resource-intensive.
- Data Inconsistency and Quality: Ensuring the consistency and quality of data across various systems is a significant challenge. Disparate data formats, incomplete data, and varying data standards can hinder effective data exchange.
- Technical Complexity: Implementing FHIR involves understanding and applying complex technical standards. This requires specialized knowledge and skills, which may not be readily available within all organizations.
- Resource Constraints: Adopting new interoperability standards often requires substantial investments in technology, training, and personnel. Limited budgets and resources can delay or impede implementation efforts.
- Regulatory Compliance: Healthcare data is subject to strict regulatory requirements, such as HIPAA in the United States. Ensuring that FHIR implementations comply with these regulations adds an additional layer of complexity.
Addressing legacy system integration
Integrating legacy systems with FHIR standards is a common hurdle. Here are some strategies to tackle this challenge:
- Incremental Integration: Instead of a full-scale overhaul, consider a phased approach to integration. Start by integrating critical systems and gradually extend to other areas.
- Middleware Solutions: Use middleware to bridge the gap between legacy systems and modern applications. Middleware can facilitate data exchange without requiring extensive changes to existing systems.
- Data Mapping and Transformation: Implement robust data mapping and transformation processes to ensure that data from legacy systems is accurately translated into the FHIR format. This preserves data integrity and usability.
Ensuring regulatory compliance
Regulatory compliance is paramount when dealing with healthcare data. Here are some steps to ensure compliance during FHIR implementation:
- Understand Regulatory Requirements: Thoroughly understand the regulatory landscape relevant to your region, such as HIPAA in the United States or GDPR in Europe. This includes knowing the specific requirements for data handling, security, and privacy.
- Implement Security Measures: Incorporate strong security measures, such as encryption, secure authentication, and regular security audits, to protect patient data. Ensure that these measures comply with regulatory standards.
- Regular Audits and Monitoring: Conduct regular audits and continuous monitoring to ensure ongoing compliance with regulatory requirements. This helps identify and address any compliance issues promptly.
Additional considerations
- Stakeholder Engagement: Engage stakeholders from the beginning to understand their needs and expectations. This includes clinicians, IT staff, administrators, and patients. Their input can guide the implementation process and improve buy-in.
- Training and Education: Provide comprehensive training and education to staff on FHIR standards and interoperability. This ensures that all team members are equipped to handle the new system effectively.
- Continuous Improvement: Treat FHIR implementation as an ongoing process. Regularly update and refine the system to keep up with evolving standards, technologies, and regulatory requirements.
Conclusion
Implementing FHIR is essential for achieving enhanced interoperability, improving patient outcomes, and boosting operational efficiency within the healthcare sector. While the process can be challenging, the benefits far outweigh the hurdles when approached with careful planning, adherence to best practices, and a strategic mindset.
Partnering with a software development company like bART Solutions, which specializes in the healthcare sector, can significantly ease the transition. Our team of experienced engineers is proficient in HL7 standards, particularly FHIR, and can assist with specific tasks or manage the entire project based on your needs.
