In the complex healthcare industry, payment models play a crucial role in determining how providers are reimbursed for their services. This article delves into the details, exploring the benefits and intricacies of various payment models and their impact on the healthcare system.
The 3 fundamental payment models in healthcare
Fee-for-Service (FFS)
Originating during the American Great Depression, the fee-for-service model is a traditional approach to healthcare payments. In this model, payments are made directly based on the amount of service patients receive, regardless of the quality of those services. Providers are compensated for each office visit, lab test, or procedure performed, creating a direct correlation between the volume of services delivered and the revenue generated.
Pros:
Simplicity: The model is straightforward and easy to understand for both providers and patients.
Increased access: Encourages physicians to see more patients, potentially reducing wait times and increasing access to care, which is critical in addressing the physician shortage, especially in primary care.
Predictability: Provides a predictable revenue stream for providers based on the volume of services rendered.
Cons:
Overutilization: May incentivize unnecessary procedures and tests, driving up healthcare costs without necessarily improving patient outcomes.
Quality concerns: Focuses on quantity over quality, which can compromise the overall standard of care.
Administrative burden: High volume of billing and claims processing can be time-consuming and costly, detracting from patient care.
Value-Based Care (VBC)
Emerging as a response to the inefficiencies of the fee-for-service model, value-based care focuses on the quality rather than the quantity of care provided. This approach gained significant traction in the early 2000s as healthcare costs continued to rise without corresponding improvements in patient outcomes.
Key components of VBC include preventive care, chronic disease management, and coordinated care. Providers are measured and compensated based on quality metrics, such as patient satisfaction, reduced hospital readmissions, and improved clinical outcomes. Programs like Medicare’s Hospital Readmissions Reduction Program (HRRP) penalize hospitals for excessive readmissions, thereby encouraging better care.
Pros:
Improved outcomes: Encourages preventive care and effective management of chronic diseases, leading to overall better health outcomes.
Cost efficiency: Aims to reduce unnecessary services and lower overall healthcare costs.
Patient-centered: Focuses on patient satisfaction and quality of care, enhancing the healthcare experience.
Cons:
Implementation costs: Requires significant investments in technology and training for data tracking and management.
Complexity: Demands a comprehensive understanding of quality metrics and performance indicators.
Risk management: Providers must manage financial risks associated with meeting performance targets.
Bundled payments
The concept of bundled payments was first introduced in the 1980s as a way to control rising healthcare costs and improve care coordination.
Bundled payment models, also known as episode-based payments, involve a single, comprehensive payment for all services provided during a patient’s entire episode of care. This could include surgery, hospitalization, and post-acute care. The objective is to encourage healthcare providers to deliver more coordinated and efficient care by aligning financial incentives across the care continuum. Success under this model relies heavily on effective communication and data sharing among all parties involved in the patient’s care .
Pros:
Care coordination: Encourages providers to collaborate, leading to more cohesive and efficient patient care.
Cost control: Helps control healthcare costs by reducing unnecessary services and improving resource allocation.
Predictable costs: Provides a clear, predictable payment structure for both providers and payers.
Cons:
Distribution complexity: Managing and distributing the bundled payment among various providers can be challenging.
Financial risk: Providers bear the financial risk if the cost of care exceeds the bundled payment amount.
Implementation challenges: Requires significant coordination and communication among different healthcare entities.
Challenges faced by Healthcare providers across various payment models
Fee-for-Service
- Financial Incentives misalignment: Providers are incentivized to increase the quantity of services rather than focusing on the quality. Such misalignment leads to overutilization of healthcare services, driving up costs without corresponding improvements in patient outcomes.
- Administrative burden: Managing a high volume of claims and billing processes is time-consuming and costly. The administrative workload is detracting from the time available for patient care, impacting overall efficiency.
Value-Based Care
- Data management: Requires robust data collection and analytics capabilities to track and report on performance metrics. Providers must invest in EHRs and data analytics tools to monitor patient outcomes and ensure compliance with quality measures.
- Initial costs: Transitioning to a value-based system can involve significant upfront investments in technology and training. These costs are a barrier for smaller practices with limited resources, making the transition challenging.
Bundled Payments
- Coordination and collaboration: Effective implementation requires seamless coordination. Providers must work together to manage patient care across different settings, such as hospitals, outpatient facilities, and rehabilitation centers.
- Risk management: Providers bear financial risk if the cost of care exceeds the bundled payment amount. This risk needs careful management of resources and adherence to evidence-based care protocols to avoid financial losses.
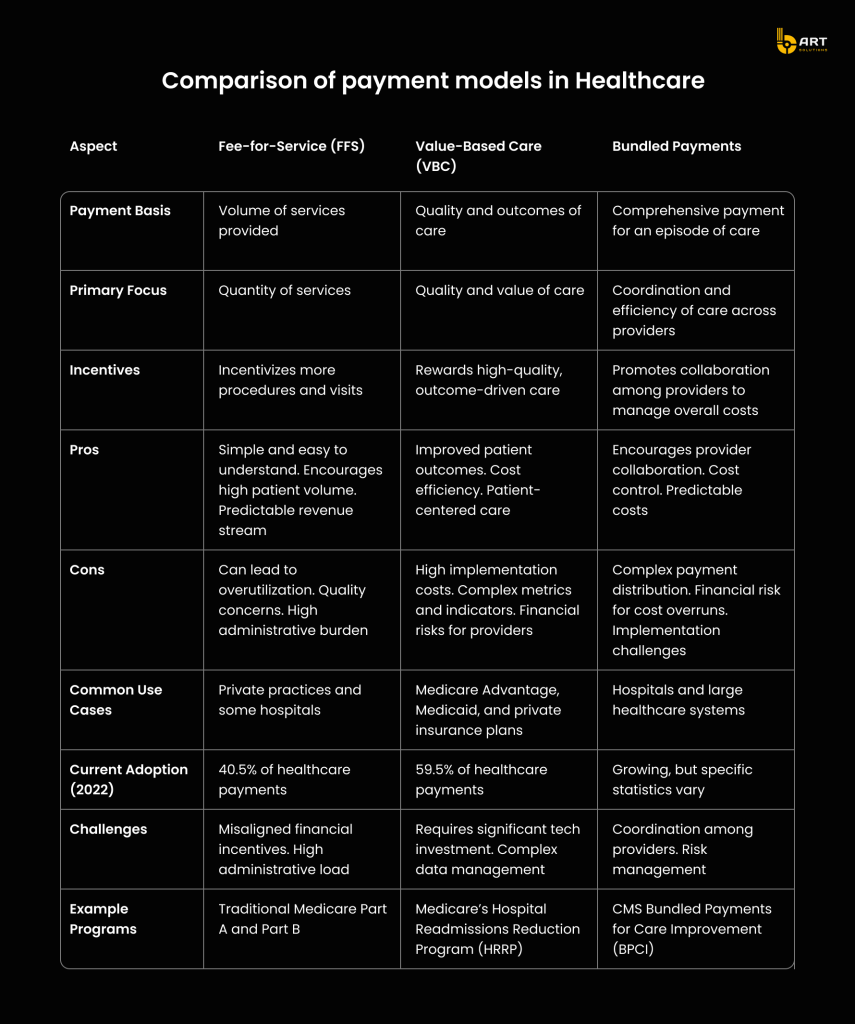
Comparison of payment models in Healthcare
To clearly understand the differences between healthcare payment models, it’s essential to compare their characteristics, benefits, and challenges side-by-side.
The impact of payment models on Healthcare IT systems
Healthcare IT systems must be robust, flexible, and capable of handling the unique demands of each payment model. Here’s a detailed look at the impact of each payment model on healthcare IT infrastructure:
Fee-for-Service (FFS)
High volume of billing and claims processing
- Automation needs: Given the high frequency of transactions under FFS, healthcare IT systems must automate billing and claims processing to handle large volumes efficiently.
- Data management: Systems must manage extensive data on individual services rendered, including patient visits, lab tests, and procedures.
Focus on RCM
- Billing software: IT systems need robust billing software that can generate, submit, and track numerous claims.
- EHR integration solutions: Seamless integration with EHRs is crucial to ensure that all services provided are accurately documented and billed.
Value-Based Care (VBC)
Advanced data analytics
- Quality metrics tracking: VBC models require IT systems capable of tracking and reporting on various quality metrics, such as patient outcomes, readmission rates, and preventive care measures.
- Predictive analytics: IT systems must incorporate predictive analytics to identify high-risk patients and intervene early.
Comprehensive data integration
- Interoperability: IT systems must support interoperability standards such as HL7 and FHIR to facilitate the integration of data from multiple sources, including hospitals, clinics, and laboratories.
- Population Health Management: Systems must aggregate and analyze data across different patient populations to identify trends, gaps in care, and opportunities for improvement.
Patient engagement tools
Patient portals and mobile apps: Enhancing patient engagement is a key component of VBC. Patient portals and mobile applications allow patients to access their health information, schedule appointments, and communicate with doctors.
Bundled Payments
Coordination and collaboration tools
- Care coordination platforms: Bundled payments require tight coordination among all parties involved in a patient’s care. IT systems must support care coordination, enable providers to share information, collaborate on treatment plans, and track patient progress.
- Shared care plans: Software should facilitate the creation and management of shared care plans that include inputs from multiple providers.
Financial management and distribution
- Bundled payment management: EHR solutions need to manage the financial aspects of bundled payments. This requires tools that can track costs, allocate scheduled payments based on pre-agreed terms, and ensure transparency in financial transactions.
- Cost tracking and reporting: Accurate tracking of costs associated with an episode of care is essential. Systems must provide detailed reports on the cost of services provided, helping providers to manage resources and identify areas for cost savings.
Risk management
- Risk adjustment models: Bundled payments involve financial risk if the cost of care exceeds the bundled payment amount. IT systems must support risk adjustment models that account for patient complexity and adjust payments accordingly.
- Outcome monitoring: Continuous monitoring of patient outcomes is crucial to ensure that care quality is maintained within the cost constraints of the bundled payment. IT systems should provide real-time dashboards and alerts to track patient progress and intervene when necessary.
The impact of payment models on healthcare IT
- Interconnected solutions: Whether operating under FFS, VBC, or bundled payments, IT systems must integrate seamlessly with EHR solutions to provide a holistic view of patient care. This interconnectedness enhances data accuracy, improves care coordination, and supports comprehensive reporting and analytics.
- Regulatory compliance: IT systems must ensure compliance with regulatory standards such as HIPAA for data security and privacy, as well as CMS guidelines for reporting and reimbursement.
- Adaptability: As healthcare payment models continue to evolve, IT systems must be scalable and flexible to adapt to new requirements. This includes the ability to incorporate new data sources, support emerging technologies, and adjust to changing regulatory landscapes.
Use cases from well-known healthcare providers
Kaiser Permanente: Integration of advanced EHR solutions to manage bundled payments
Kaiser Permanente operates a comprehensive healthcare system that includes hospitals, outpatient facilities, and a large network of physicians. This integrated structure is ideal for implementing bundled payments, where a single payment is made for all services related to a specific treatment.
Kaiser utilizes an advanced EHR and CRM system called KP HealthConnect, one of the largest private electronic health records in the world. It integrates patient information across all care settings, enabling seamless access to medical records for all professionals involved in a patient’s care.
Key benefits
- Integration across providers: KP HealthConnect ensures that all healthcare providers, including primary care physicians, specialists, and hospital staff, have access to the same patient information. This integration facilitates coordinated care, essential for the success of bundled payments.
- Tracking and reporting: By analyzing data on patient care pathways, Kaiser can identify inefficiencies and areas for improvement, ensuring that care is delivered within the cost constraints of the bundled payment while maintaining high-quality standards.
- Patient portals: Through these portals, patients can access their medical records, schedule appointments, and communicate with their healthcare providers. Engaging patients in their care journey is crucial for the success of bundled payments, as it helps ensure adherence to care plans and follow-up visits, reducing the risk of complications and readmissions.
- Efficient resource utilization: By leveraging the integrated EHR solution, Kaiser Permanente can closely monitor the resources used during a patient’s care episode. Such monitoring helps prevent unnecessary tests and procedures, aligning with the goals of bundled payments to reduce costs without compromising care quality.
Mayo Clinic: Leading the way in value-based care
Mayo Clinic, a global leader in medical care, research, and education, has been at the forefront of implementing VBC models to enhance healthcare delivery.
Key benefits
- Collaborative approach: Mayo Clinic employs a team-based approach to healthcare. This ensures that each patient receives comprehensive and coordinated treatment, addressing all aspects of their health.
- Advanced analytics: Mayo Clinic leverages advanced data analytics to monitor and evaluate patient outcomes. Their use of predictive analytics helps in identifying high-risk patients and intervening early to prevent complications.
- Outcome tracking: Advanced data analytics tools support continuous tracking of clinical outcomes and allow Mayo Clinic to refine their treatment protocols and improve care quality.
- Patient portals and apps: Mayo Clinic provides patients with access to their health information through online portals and mobile apps. These tools empower patients to take an active role in their healthcare, enhancing adherence to treatment plans and improving satisfaction.
Cleveland Clinic: Utilizing innovative technologies
Cleveland Clinic is renowned for its cutting-edge medical research, top-tier patient care, and educational initiatives. With a strong focus on leveraging technology, Cleveland Clinic has implemented numerous innovative solutions to enhance healthcare efficiency and quality.
Key benefits
- Virtual visits: Cleveland Clinic has significantly expanded its telehealth services, offering virtual visits to patients across various specialties.
- Remote patient monitoring: By using wearable devices and remote monitoring systems, Cleveland Clinic tracks patients’ vital signs and health metrics in real-time.
- Predictive analytics: Cleveland Clinic employs AI and ML algorithms to analyze vast amounts of patient data.
- Clinical decision support: By providing evidence-based recommendations, these systems enhance clinical accuracy and patient safety.
- Collaborations with tech companies: Cleveland Clinic has partnered with leading technology companies like IBM and Google to develop innovative healthcare solutions. For example, their partnership with IBM Watson Health leverages AI to improve cancer care by analyzing clinical data and providing treatment options.
- Interoperable systems: Cleveland Clinic has optimized its EHR systems to ensure seamless data exchange across different healthcare settings.
- Patient portals: The clinic’s EHR system includes patient portals that allow patients to access their health records, communicate with providers, and manage appointments.
Intermountain Healthcare: Enhancing VBC through comprehensive data analytics
Intermountain Healthcare operates a network of hospitals, clinics, and other healthcare services. Known for its focus on clinical excellence and innovation, Intermountain has integrated data analytics into its value-based care strategy to drive better health outcomes and cost efficiency.
Key benefits
- Enterprise Data Warehouse (EDW): Intermountain Healthcare has developed an extensive Enterprise Data Warehouse that aggregates data from various sources, including EHRs, billing systems, and clinical databases. This centralized data repository supports comprehensive analysis and reporting.
- Interoperability: Ensuring data interoperability across different systems allows seamless data exchange, enabling a holistic view of patient care and facilitating coordinated efforts across care teams.
- Risk stratification: Intermountain uses predictive analytics to stratify patients based on risk, identifying those who are at higher risk for adverse health outcomes.
- Population health tools: Analytics tools help in managing population health by tracking health metrics, monitoring chronic diseases, and identifying gaps in care.
- Evidence-based guidelines: Intermountain’s CDSS integrates evidence-based guidelines into clinical workflows, providing real-time decision support to clinicians.
- Cost management: Financial analytics tools are used to monitor healthcare costs and identify areas for cost reduction without compromising quality.
- Value-Based contracting: Intermountain leverages financial analytics to negotiate value-based contracts with payers, aligning financial incentives with care quality and patient outcomes.
Healthcare IT challenges
Integrating diverse payment models in healthcare IT involves navigating several technical challenges, including managing complex data, ensuring interoperability, and maintaining data privacy and security. Addressing these challenges is crucial for healthcare organizations to optimize their revenue cycles, improve patient outcomes, and comply with regulatory requirements.
Each payment model has unique requirements and workflows that must be accommodated within the EHR system.
Fee-for-Service (FFS)
High transaction volume: FFS models generate a high volume of transactions due to the billing of individual services. EHR systems must be capable of handling and processing numerous claims efficiently.
Detailed service tracking: Accurate tracking and documentation of each service rendered are essential for billing purposes, requiring robust EHR functionalities.
Value-Based Care (VBC)
Quality and outcome metrics: VBC models rely on detailed tracking of quality metrics and patient outcomes. EHR systems must integrate these metrics into clinical workflows and provide analytics tools to measure performance.
Risk adjustment and stratification: EHRs must support complex algorithms for risk adjustment and patient stratification to align with VBC incentives.
Bundled Payments
Comprehensive episode management: Bundled payment models require tracking the entire episode of care across multiple providers and settings. EHR systems must ensure seamless data flow and coordination among all involved parties.
Cost and resource allocation: Accurate allocation of costs and resources across the care continuum is crucial, requiring sophisticated financial management tools within the EHR.
Data management challenges
Data accuracy
- Consistent data entry: Inconsistent data entry practices lead to inaccuracies that affect billing and reporting. EHR systems must implement standardized data entry protocols and validation checks.
- Real-time data updates: Payment models, especially VBC, require real-time data updates to track patient outcomes and performance metrics accurately. Healthcare IT infrastructure must support real-time data synchronization across different modules.
Data privacy and security
- Compliance with regulations: EHR systems must comply with stringent regulations such as HIPAA to protect patient data. This includes implementing robust encryption, access controls, and audit trails.
- Risk of data breaches: EHR systems must employ advanced security measures, such as multi-factor authentication and intrusion detection systems, to safeguard sensitive information.
Interoperability issues
Interoperability, or the ability of different EHR systems and payment databases to exchange and use information seamlessly, remains a significant challenge.
Standardization of data formats
- Lack of uniform standards: The healthcare industry lacks uniform standards for data exchange, leading to compatibility issues between different EHR systems and payment databases.
- Custom interfaces: Many EHR systems require custom interfaces to communicate with other systems, increasing complexity and maintenance costs.
Integration with external systems
- Multiple vendors: Healthcare organizations often use EHR systems from multiple vendors, each with its own data formats and communication protocols. Ensuring interoperability between these systems is a complex task that requires careful planning and execution.
- Payment databases: Integrating payment databases with EHR systems involves synchronizing financial data with clinical data. This requires robust APIs and middleware solutions to facilitate data exchange.
Best practices for mapping payment models to EHR systems

Understanding payment model requirements
- Fee-for-Service (FFS): Focus on accurate service documentation and efficient claims processing. Ensure EHR systems support detailed coding and billing functionalities to handle the high volume of transactions.
- Value-Based Care (VBC): Emphasize tracking of quality metrics, patient outcomes, and risk stratification. EHR systems should integrate tools for measuring performance against value-based benchmarks and facilitate data-driven decision-making.
- Bundled Payments: Manage comprehensive care episodes, requiring coordination across multiple providers. Ensure EHR systems support episode-based documentation, cost tracking, and resource allocation.
Aligning EHR functionalities with payment model needs
- Custom workflows: Develop custom workflows within the EHR to match the specific needs of each payment model. For example, creating specialized templates for documenting chronic disease management in VBC or integrated care pathways for bundled payments.
- Integrated financial management: Ensure that EHR systems include financial management modules capable of handling diverse payment structures, from individual service billing in FFS to bundled payments that cover an entire episode of care.
Ensuring data integrity and accessibility
- Real-time data access: Implement systems that provide real-time access to patient data. This is crucial for VBC models where timely interventions can significantly impact patient outcomes.
- Data validation and standardization: Use standardized data entry protocols to ensure consistency and accuracy. Implement validation rules to prevent errors and maintain data integrity.
Enhancing interoperability
- Health Information Exchanges (HIEs): Participate in HIEs to facilitate seamless data exchange across different healthcare systems.
- Standard protocols: Adopt industry standards such as HL7 and FHIR to enhance interoperability between EHR systems and external databases.
Facilitate integration
Several technologies and tools can facilitate the integration of diverse payment models with EHR systems:
- Standardized APIs: Utilize standardized APIs like those based on the FHIR protocol to enhance interoperability and data sharing across different healthcare platforms.
- Integration middleware: Implement middleware solutions that act as intermediaries between disparate systems, translating data formats and ensuring compatibility.
- Cloud-based middleware: Cloud middleware can handle large volumes of data and support real-time processing, essential for modern healthcare environments.
- Predictive analytics: Incorporate predictive analytics tools to identify high-risk patients and optimize care pathways.
- Automated billing: Implement EDI solutions to automate billing and claims processing. EDI ensures accurate and timely submission of claims, essential for FFS models.
- Patient portals: Integrate patient portals with EHR systems to enhance patient engagement.
- Mobile health apps: Develop mobile health apps that connect to EHR systems, providing patients with real-time access to their health data and personalized health management tools.
- Encryption solutions: Use advanced encryption technologies to protect patient data during transmission and storage.
- Access control systems: Multi-factor authentication and audit trails enhance security and ensure only authorized personnel can access sensitive information.
Future trends and innovations

Shift towards value-based care
Value-based care models will become more prevalent as healthcare providers and payers seek to align financial incentives with patient outcomes. This shift will require EHR systems to integrate advanced technologies for analytics and quality tracking.
Expansion of bundled payments
Bundled payment models are expected to expand beyond traditional areas like orthopedics and cardiology to include more complex care episodes and chronic disease management. EHR systems will support more sophisticated episode-based tracking and cost management features.
Emerging technologies that could streamline integration
Several emerging technologies have the potential to further streamline the integration of payment models with EHR systems, enhancing efficiency and improving financial outcomes:
Blockchain: Blockchain can provide a secure and transparent way to share patient data across different healthcare providers. Its decentralized nature ensures data integrity and reduces the risk of data breaches. Smart contracts on blockchain can automate payment processing and claims management, ensuring timely and accurate reimbursement based on predefined criteria.
Artificial Intelligence and Machine Learning: AI and ML can predict patient outcomes and identify high-risk patients, enabling proactive interventions. These technologies can also optimize resource allocation and reduce unnecessary procedures.
NLP technologies can enhance EHR systems by enabling the extraction of meaningful information from unstructured data, such as clinical notes, to support better decision-making and improve documentation accuracy.
Internet of Things (IoT): IoT devices can continuously monitor patients’ health metrics and integrate this data into EHR systems. Real-time data flow supports value-based care models by enabling timely interventions and personalized care.
Advanced Analytics and Big Data: Advanced analytics can analyze large datasets to identify trends, track population health metrics, and develop targeted interventions.
Big data analytics can provide real-time insights into patient care processes, helping healthcare providers to make data-driven decisions and optimize care delivery.
The role of policy and regulation in shaping the future of healthcare payments

Policy and regulation play a critical role in shaping the future of healthcare payments and IT systems. Key areas of influence include:
Government Programs: Initiatives like the Medicare Access and CHIP Reauthorization Act (MACRA) and the Merit-based Incentive Payment System (MIPS) encourage the adoption of value-based care models. These programs require EHR systems to support quality reporting and performance tracking.
Funding and Grants: Government funding and grants for health IT innovation accelerate the development and adoption of advanced technologies, such as AI and blockchain, in healthcare.
Pilot Programs: Regulatory bodies support pilot programs that test new payment models and tools, paving the way for broader implementation of advanced EHR systems.
Summary
Choosing the right payment model for your practice is ultimately your decision, but we’re here to support you every step of the way. Once you’ve evaluated the pros and cons of various healthcare payment models, the next step is to select the best software for your practice.
That’s where bART Solutions comes in. We will provide expert guidance and develop custom software tailored to your specific needs and budget.
Connect with us, and our project managers will help you refine your options, and our development team will start crafting the perfect software solution for your practice.