In the rapidly evolving healthcare industry, efficiency and patient care hinges on the quality and performance of Electronic Health Record (EHR) systems.
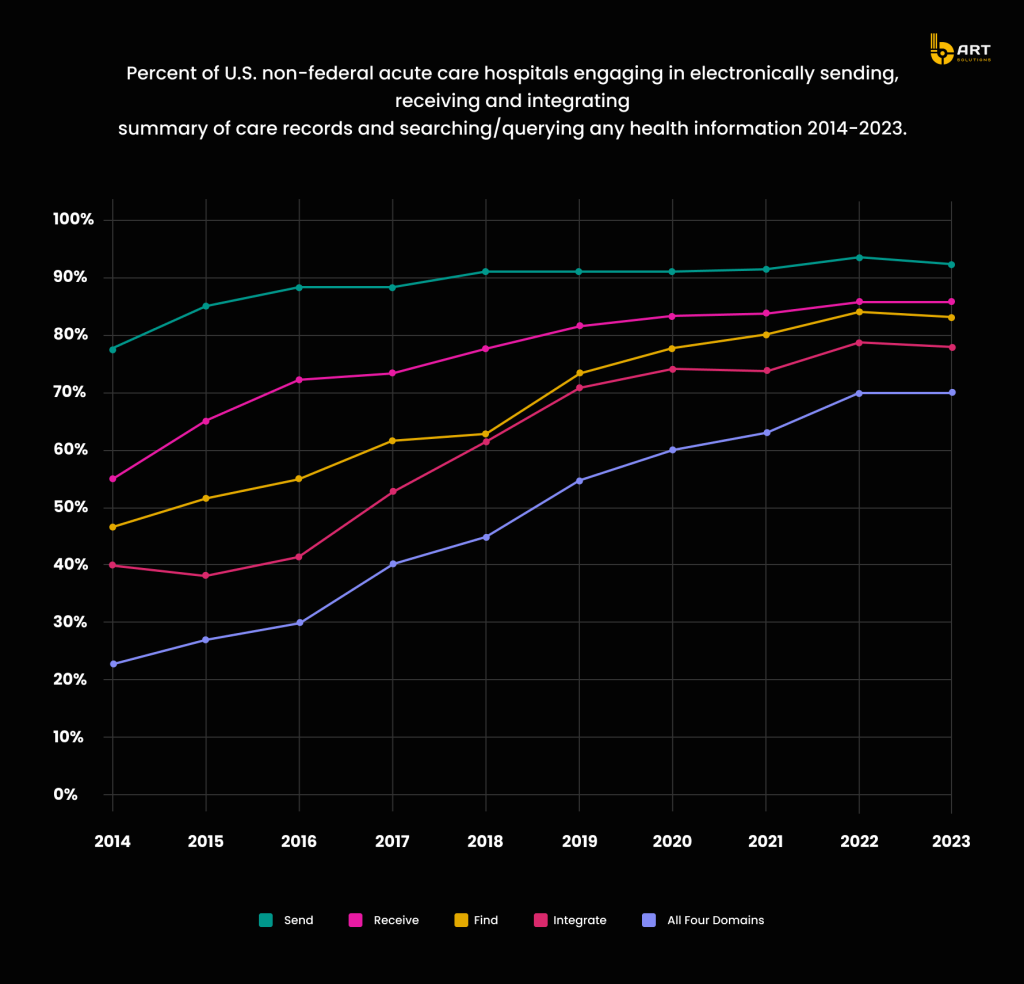
According to the American Hospital Association Information Technology Supplement, hospital engagement in interoperable exchange has significantly improved, with 70% of hospitals engaging in all four measured interoperability domains — sending, receiving, finding, and integrating health information — from 2021 to 2022. Between 2022 and 2023, hospital engagement in each activity remained stable, but it’s projected to grow further in the future because of the ongoing need for efficient data exchange and the push towards comprehensive, integrated healthcare solutions.
Outdated EHR systems clearly become barriers to effective patient care, introducing inefficiencies and increasing the likelihood of errors. By identifying these issues, organizations can better grasp the need for healthcare IT modernization and the benefits of legacy EMR or EHR system upgrade.
The Pitfalls of Using Outdated EHR Solutions
Mainframe-Based EHR Systems: Many legacy EHR systems are built on mainframe technology, which, while robust, lacks the flexibility of modern systems. These mainframes often struggle with interoperability, making it difficult to integrate with external labs or imaging centers, leading to delays in receiving patient information.
Client-Server Architectures: Older EHR platforms rely on client-server architectures that are expensive to maintain and difficult to scale. In contrast, cloud-based EHR systems offer enhanced scalability, cost-effectiveness, and reliability.
Proprietary Data Formats: An EHR system that stores data in a unique format may require custom-built solutions for data extraction and migration, increasing both the time and cost of the process.
Limited Mobile Access: Lack of mobile accessibility hinders healthcare providers’ ability to access patient data on the go. For example, a physician unable to review patient records remotely may not have the necessary information during an emergency, affecting the quality of care provided.
Inadequate User Interfaces: Older EHR systems often feature cumbersome and non-intuitive user interfaces. A system that requires multiple clicks and complex navigation for simple tasks can lead to user frustration and decreased productivity. This also results in higher training costs and longer onboarding times for new staff.
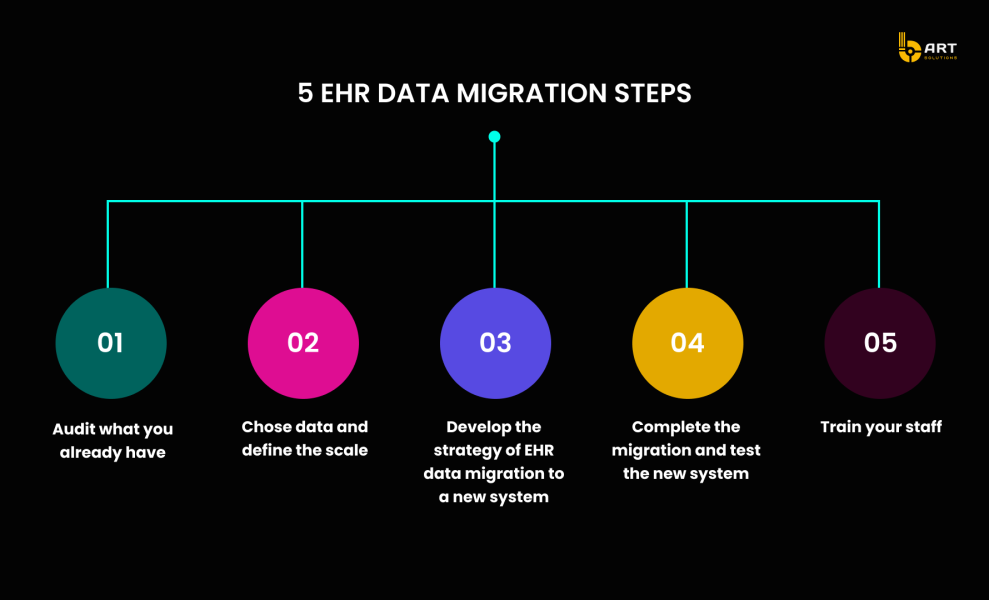
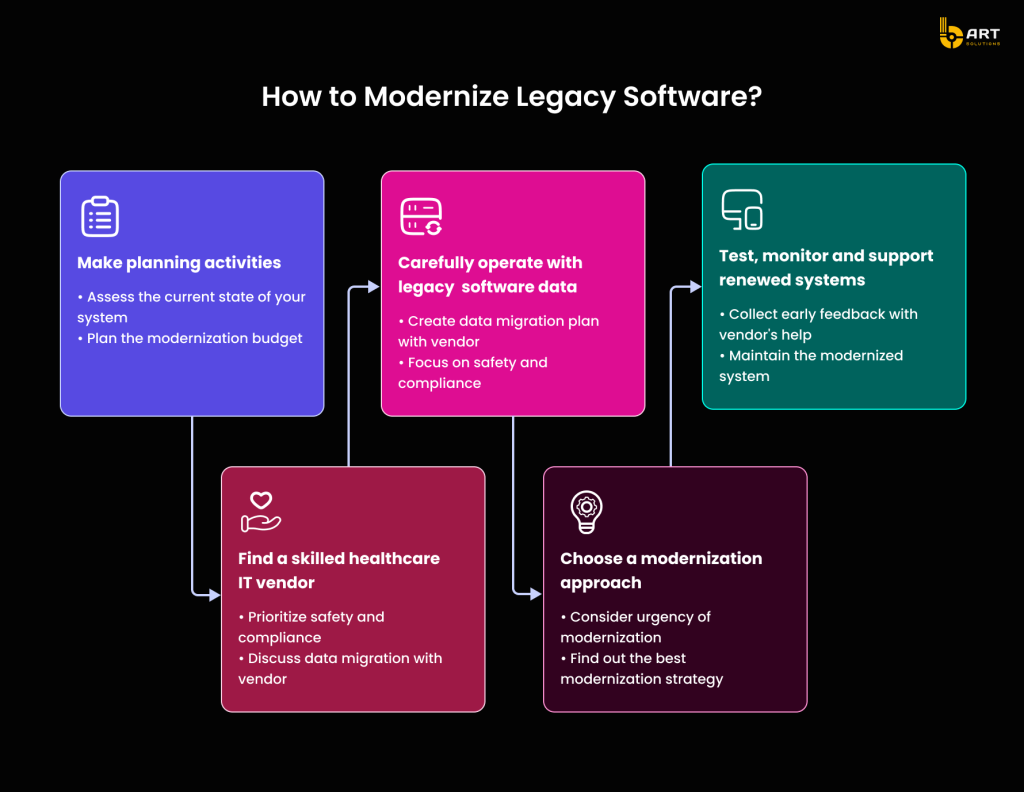
Pre-Migration Planning
Comprehensive planning helps mitigate risks, meet stakeholder needs, and achieve desired outcomes without disrupting ongoing healthcare operations.
Strategic Stages of Pre-Migration Planning
- Comprehensive Approach to Legacy EHR Data Extraction: Before migrating data from a legacy EHR system to a new platform, conducting a thorough data assessment is essential. This involves evaluating the current data landscape, focusing on data volume, types, and quality.
- Data Volume Assessment: Conduct an inventory of all existing data and categorize it before migration; review patient records, appointment schedules, billing information, and other relevant datasets. Estimating the total volume of data to be migrated helps in developing the necessary infrastructure and resources for the process. A study by ScienceDaily investigating the use cases of optimized EHR data demonstrated a productivity boost of 15%.
- Handling Critical Data: Identify clinical data required for ongoing patient care, regulatory data for compliance with HIPAA and GDPR, and operational data for daily activities such as scheduling and billing.
EHR Data Mapping and Normalization
Data mapping ensures accurate data migration and transformation for an upgraded healthcare solution. Normalization secures consistency and accuracy in patient records, enabling seamless data exchange across different healthcare solutions.
Standardizing Data Formats: Convert data into standardized formats by mapping disparate data elements to universal codes and terminologies, such as ICD-10 for diagnoses and SNOMED CT for clinical terms.
Data Cleansing: Identify and correct errors, inconsistencies, and duplicates to maintain data integrity. Use data quality tools to flag anomalies and ensure only accurate data is migrated to the new EHR system.
Data Enrichment: Enhance data with additional context or details to improve its usability. Adding missing demographic information or linking patient records with relevant clinical guidelines provides a comprehensive view of patient health.
Regular Audits and Validation: Continuous monitoring and validation ensure the normalization process is effective and all data remains accurate over time.
Importance of Stakeholder Engagement in EHR Migration
Involving stakeholders early in the migration process ensures that the new EHR system meets operational needs and gains user acceptance.
Insights from Key Stakeholders in EHR Migration
- Clinicians: Gathering insights from clinicians about their daily workflows ensures that the new system supports and enhances clinical efficiency.
- IT Staff: Collaborating with IT staff is essential to understand the technical requirements for system integration, data migration, and ongoing maintenance.
- Administration: Collecting requirements from administrative staff ensures the new system supports billing, scheduling, and reporting functionalities. Meeting regulatory compliance and reporting standards during the EHR migration addresses administrative needs effectively.
Effective Requirement Gathering
Conduct workshops and interviews with structured questionnaires to ensure comprehensive coverage of all relevant aspects. Develop use cases based on gathered requirements to validate and prioritize system features. Create prototypes of new system features and collect feedback to refine requirements and meet user expectations.
Ensuring Secure and Efficient EHR Data Migration
Automated EHR data migration ensures precise data mapping and conversion, significantly reducing errors and manual effort. By automating complex tasks such as data extraction, transformation, and loading, healthcare providers can swiftly manage vast amounts of information while preserving data integrity and adhering to HIPAA regulations.
Examination of EHR Migration Challenges and Remedies
Modernizing EHR systems involves several risks that must be identified and addressed to ensure a smooth transition.
- Data Loss: Implement robust backup strategies to ensure no data is lost, including regular backups and verification processes.
- Downtime: Plan migration activities during off-peak hours to minimize operational impact. Develop a detailed timeline and communicate it effectively to all stakeholders.
- Compatibility Issues: Conduct thorough testing to ensure the new EHR system is compatible with all existing components. This helps identify and address potential issues before full-scale implementation.
Developing a EHR Migration Project Plan
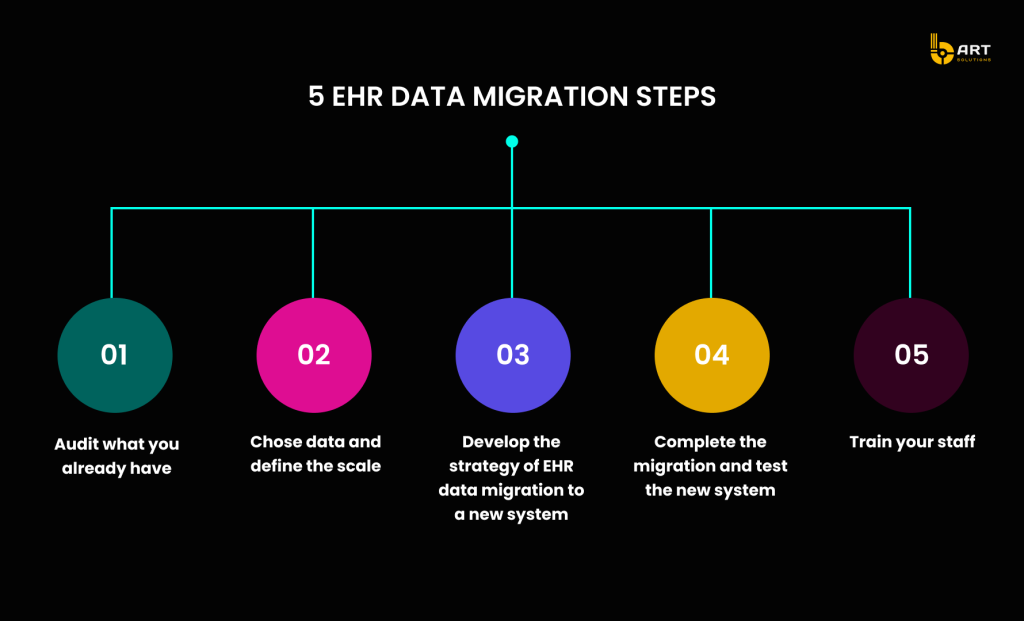
EHR migration best practices suggest starting with a comprehensive risk mitigation plan to ensure a smooth transition from legacy EHR systems to modern platforms. This roadmap should address potential issues through thorough contingency planning, regular testing, and robust support mechanisms.
EHR Migration Project Plan Components
- Fallback Procedures: Develop procedures to handle system failures or data corruption. A rollback plan helps revert to the legacy system if needed, ensuring continuous operation and data integrity.
- Pilot Testing: Conduct pilot migrations to fine-tune processes and address unforeseen problems, reducing the risk of pitfalls during the actual migration.
- Post-Migration Data Validation: Implementing post-migration data validation checks ensures all data has been accurately migrated and the new EHR system functions as expected.
Training and Support
Effective training reduces resistance to change and enhances productivity by helping users become proficient with the new tools and workflows. Training should cover all aspects of the new system, including navigation, data entry, and reporting.
User Training Programs: Ensure comprehensive training programs to reduce errors and increase productivity.
Support Mechanisms: Establish help desks and provide online resources, including training materials, FAQs, and troubleshooting guides, to support continuous learning and problem-solving.
User Feedback Mechanisms: Gather user input to identify areas for improvement and ensure the system evolves to meet user needs.
For assistance in modernizing complex medical solutions like EHR/EMR safely and efficiently, contact the expert team at bART Solutions.
Guidelines for Selecting Between EHR Migration Strategies
Choosing the right migration strategy involves assessing factors such as the complexity of the data, the need for continuous operations, resource availability, regulatory compliance, and the organization’s risk tolerance.
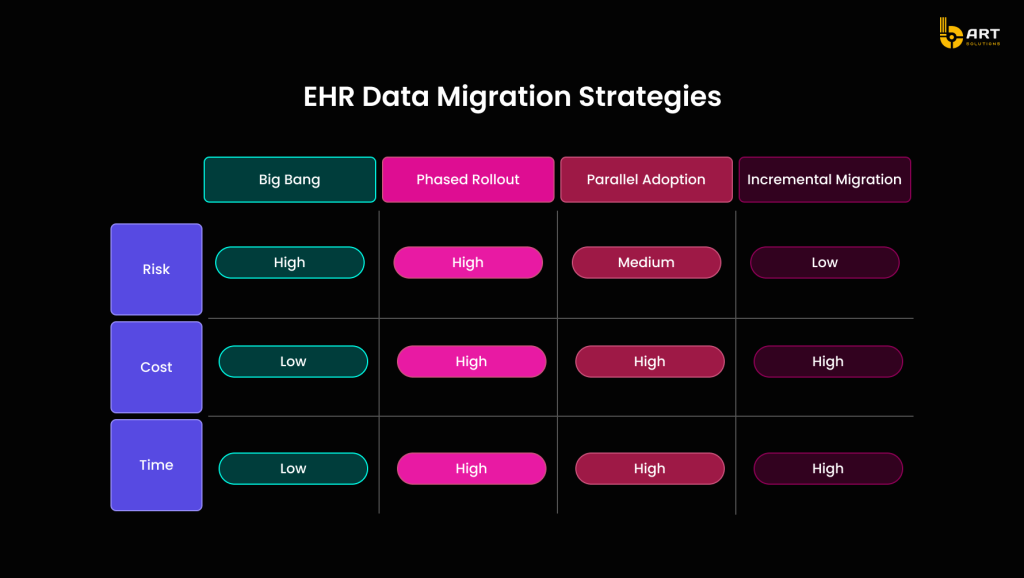
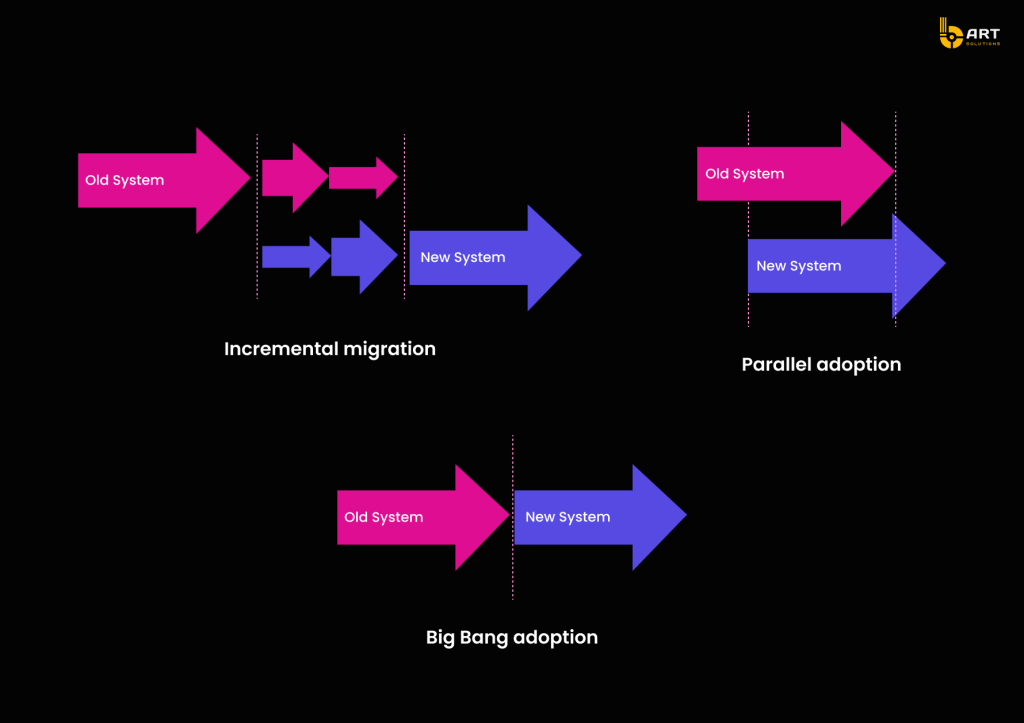
Big Bang vs. Phased EHR Migration
Big Bang EHR Migration
The Big Bang approach involves migrating all data and transitioning to the new system in a single, large-scale operation. This method requires significant preparation and a short period of intense activity where the old system is entirely replaced by the new one.
Pros
- Short Transition Period: The transition happens quickly, minimizing the period of dual operation.
- Immediate Benefits: All new system features and improvements are available immediately after the migration.
Cons
- High Risk: If issues arise, they can be catastrophic since the entire system relies on a successful migration.
- Significant Downtime: A considerable downtime may occur during the switch-over.
- Resource Intensive: Requires substantial resources and coordination to execute effectively.
Phased EHR Migration
Phased EHR migration involves gradually transferring data and functionalities to the new system over a period of time. This approach allows for parts of the system to be tested and validated before full implementation.
Pros
- Reduced Risk: Problems can be identified and resolved in smaller, manageable segments.
- Less Disruption: Minimizes operational disruption by allowing continued use of the old system during the migration process.
- Flexibility: Easier to adjust the migration plan based on feedback and issues encountered.
Cons
- Extended Transition Period: The migration process takes longer, potentially leading to prolonged periods of dual operation.
- Complexity: Managing two systems simultaneously can be complex and resource-intensive.
Parallel Run or Incremental EHR Migration
Parallel Run
Parallel Run is a migration strategy where both the old (legacy) and new systems run simultaneously for a specific period. This approach ensures that the new system is functioning correctly before completely decommissioning the old one. During the parallel run, data is processed in both systems, and results are compared to ensure accuracy and consistency. This method provides a safety net, allowing organizations to identify and rectify issues in the new system without interrupting operations.
Pros
- Safety Net: Maintains operational continuity by ensuring the old system is available if the new system encounters issues.
- Validation: Allows real-time comparison and validation of data between the two systems, ensuring data integrity and reliability.
Cons
- Resource Intensive: Requires maintaining and supporting both systems simultaneously, which can be costly and labor-intensive.
- User Confusion: Users may experience confusion and increased workload from operating both systems.
Incremental Migration
Incremental Migration involves gradually transferring data and functionalities from the old system to the new one in smaller, manageable segments. This approach allows for thorough testing and validation at each stage, reducing the risk of significant disruptions during the migration process. Incremental migration is particularly beneficial for large-scale systems where a complete switchover would be too risky or impractical.
Pros
- Manageable Segments: Data is migrated in smaller, more manageable parts, allowing for detailed testing and validation.
- Continuous Improvement: Feedback from each phase can be used to improve subsequent phases, ensuring a smoother overall transition.
Cons
- Extended Timeline: The overall migration process can take significantly longer, which may prolong periods of dual operation.
- Consistency Challenges: Ensuring consistency between the old and new systems throughout the migration process can be challenging.
Using Middleware and Data Conversion Tools
Once a migration strategy is chosen, the implementation phase requires robust tools to facilitate data transfer and integration. Middleware acts as an intermediary that manages data flow between the old and new systems, ensuring data integrity and consistency throughout the migration. Data bridging tools further support this by handling complex transformations and providing seamless connectivity.
Examples of Data Conversion and Bridging Tools

Apache Camel
An open-source integration framework that allows developers to define routing and mediation rules using Java or XML. It supports a variety of data formats and communication protocols, making it a versatile choice for data bridging during migration.
Mirth Connect
Specifically designed for healthcare data integration, Mirth Connect supports the exchange of clinical and administrative data. It is widely used for connecting EHR systems and ensures secure and reliable data transfer.
Talend
A powerful data integration tool that provides capabilities for complex data transformations and migrations. Talend offers robust data quality and governance features, ensuring that data is accurate and consistent across systems.
Dell Boomi
A cloud-based integration platform that connects applications and data across various environments. Dell Boomi simplifies the integration process with pre-built connectors and an intuitive drag-and-drop interface.
Informatica
Known for its comprehensive data integration solutions, Informatica provides tools for data migration, transformation, and management. It supports complex data workflows and ensures high data quality and consistency.
Jitterbit
This integration platform allows businesses to quickly connect applications, data, and devices with pre-built templates and connectors. Jitterbit’s user-friendly interface makes it easy to automate data flows and ensure seamless integration.
Technical Considerations
EHR system modernization requires careful attention to technical aspects to ensure a secure, efficient, and compliant transition. These considerations are vital for protecting patient data, maintaining system performance, and ensuring interoperability with existing healthcare IT infrastructure.
Data Security
Implement strict access control and robust encryption methods. Utilizing secure transfer protocols such as HTTPS, SFTP, and FTPS can further safeguard data by providing encrypted channels for transmission.
Maintaining Compliance
HIPAA Compliance: Ensuring HIPPAA-compliant EHR migration is mandatory for healthcare organizations in the United States. This involves safeguarding Protected Health Information (PHI) through appropriate administrative, physical, and technical measures.
GDPR Compliance: For organizations operating in the European Union, compliance with the General Data Protection Regulation (GDPR) is essential. This regulation mandates strict data protection and privacy standards for handling personal data.
EHR Migration Performance and Downtime Management
Strategies to Minimize Downtime
Scheduled Migrations: Planning migration activities during off-peak hours can significantly reduce the impact on daily operations. This approach helps in maintaining continuity of care and minimizing disruptions.
Incremental Migration: As discussed earlier, migrating data in smaller, manageable segments can help manage and reduce downtime. Phased approach allows for testing and validation at each stage, ensuring a smoother transition.
Performance Monitoring and Load Testing
Load Testing: Conducting load tests can help identify potential performance bottlenecks in the new system. This involves simulating high-traffic conditions to ensure the system can handle peak loads without compromising performance.
Performance Monitoring: Implementing real-time performance monitoring tools can help track system performance during and after EHR migration. These tools provide insights into system health, identify issues early, and ensure that the new system meets expectations.
Integration with Existing Systems
Compatibility tests ensure that the new EHR system integrates seamlessly with existing healthcare IT systems, such as laboratory information systems (LIS), billing systems, and radiology information systems (RIS). Adopting interoperability standards such as HL7 (Health Level Seven) and FHIR (Fast Healthcare Interoperability Resources) facilitates seamless data exchange between disparate systems.
For expert guidance on developing regulatory-compliant EHR platforms, contact the experienced team at bART Solutions.
Post-Migration Activities
After migrating to a new EHR system, several critical activities ensure the transition’s success and the system’s ongoing performance. Here’s how to manage these essential steps effectively.
Data Validation and Integrity Checks
Ensuring data integrity and usability post-migration is paramount. Here are key methods and tools to validate migrated data:
Methods for Validating Migrated Data:
Record Comparison: Compare records from the old and new systems to ensure accurate data transfer.
Checksum Verification: Utilize checksum algorithms to verify data integrity during the migration. This helps detect any alterations or corruption by comparing source and destination values.
Reconciliation Reports: Generate reports to highlight discrepancies between the old and new systems. These reports help identify and correct any migration issues.
Tools for Automated Integrity Checks
- Talend Data Quality: Provides data profiling, cleansing, and validation features, ensuring post-migration data accuracy and consistency.
- Informatica Data Quality: Offers robust validation and integrity checks to maintain high data quality standards.
- IBM InfoSphere QualityStage: Validates and cleanses data, providing automated checks to ensure migrated data meets required standards.
User Training and Support
Effective user training and support are vital for a smooth transition and long-term success.
User Proficiency: Comprehensive training programs ensure that end-users are proficient in the new system, reducing errors and increasing productivity.
Smooth Transition: Well-trained users are more likely to embrace the new system, leading to a smoother transition and higher satisfaction rates.
Providing Ongoing Support and Resources
- Help Desks: Establish help desks to provide immediate assistance for users encountering issues or questions.
- Online Resources: Maintain an online repository of training materials, FAQs, and troubleshooting guides to support continuous learning and problem-solving.
- User Feedback Mechanisms: Implement feedback mechanisms to gather user input and identify areas for improvement.
Continuous Monitoring and Optimization
Continuous monitoring and optimization ensure that the new EHR system operates efficiently and evolves to meet organizational needs over time.
Establishing a Framework for Continuous Monitoring
Real-Time Monitoring: Use real-time monitoring tools to track system performance, identify issues, and ensure efficient operation.
Scheduled Audits: Conduct regular system audits to assess performance, security, and compliance.
Techniques for Ongoing Optimization and Performance Improvements
Performance Tuning: Regularly review and adjust system configurations to optimize performance. This includes optimizing database queries, adjusting server settings, and managing system resources.
User Feedback Integration: Continuously gather and integrate user feedback to identify and implement improvements, ensuring the system evolves to meet user needs and organizational goals.
Software Updates: Keep the system up-to-date with the latest software patches and updates to improve functionality, security, and performance.
By focusing on these post-migration activities, healthcare organizations can ensure the continued success and efficiency of their new EHR systems. For expert assistance in these areas, contact the experienced team at bART Solutions.
Conclusion
Migrating from legacy EHR systems to modern platforms is a critical step for healthcare organizations seeking to enhance operational efficiency, data security, and patient care quality. This comprehensive process requires careful planning and execution across various stages, from pre-migration preparation to post-migration validation.
Effective pre-migration planning ensures a smooth transition by thoroughly assessing data, engaging stakeholders, and addressing potential risks. Choosing the right migration strategy, whether it be Big Bang, Phased, Incremental, or Parallel Run, is essential for aligning with the organization’s specific needs and constraints. Technical considerations, including data security, compliance, performance management, and system integration, are crucial for maintaining the integrity and functionality of the new EHR system.
Post-migration activities, such as data validation, user training, and continuous system optimization, are vital for the long-term success and efficiency of the new system. These efforts ensure better outcomes for both providers and patients.
EHR system modernization benefits include:
- Enhanced Data Accuracy: Modern EHR systems reduce errors through improved data entry interfaces and automated checks.
- Improved Interoperability: Seamless integration with other healthcare systems and standardized data formats facilitates better information exchange.
- Streamlined Workflows: Advanced features like automated scheduling, electronic prescribing, and integrated billing systems save time and reduce administrative burdens.
- Increased User Satisfaction: Intuitive interfaces and mobile accessibility improve the user experience for healthcare providers, allowing them to focus more on patient care.
- Regulatory Compliance: Modern systems are designed to meet current regulatory standards, ensuring compliance with HIPAA, GDPR, and other relevant regulations.
- Scalability: Cloud-based EHR solutions offer scalability to accommodate growing data volumes and expanding healthcare practices.
For expert guidance and support in modernizing complex medical solutions like EHR/EMR, contact the experienced team at bART Solutions, who can help ensure a safe, efficient, and effective transition.